- Locations
- Find a Physician
- By Physician
- By Department
- The Center for Spine Health
- Hand & Wrist Center
- Shoulder & Elbow Center
- Foot & Ankle Center
- Joint Replacement Center
- The Sports Medicine Center
- Pediatric Orthopedic Center
- Trauma & Fracture Center
- Osteoporosis and Bone Health
- Oncology Center
- Cartilage Repair Center
- Concussion Rehab Center
- OrthoDirect
- Careers
- Patient Portal
- Intranet
![]() Overview | Causes | Symptoms | Diagnosis | Treatment | FAQ
Overview | Causes | Symptoms | Diagnosis | Treatment | FAQ
Overview
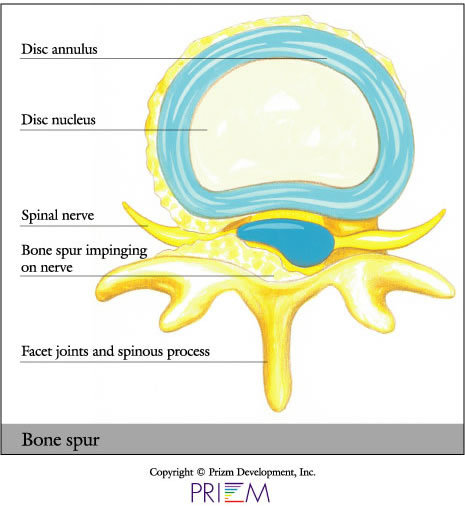
A bone spur, or osteophyte, is an excess growth of bone around a vertebral body. Bone spurs are fairly common in people over the age of 60. It is not the bone spur itself that is the real problem; pain and inflammation begin to occur when the bone spur rubs against nerves and bones. If bone spurs grow too much, they can impinge on nerve roots.
Causes
As we age, the discs in our spine naturally degenerate and lose some of their natural shock-absorbing ability. Factors that contribute to and accelerate this process include stress, injury, poor posture, poor nutrition, and family history.
It is not uncommon for people with osteoarthritis to
get bone spurs. Osteoarthritis is a degenerative condition in which
joint cartilage begins to wear down, causing bone to rub against bone.
As a result, the body may begin to produce new bone to protect against
this, which is how a bone spur forms.
[Top]
Symptoms
- Back pain and neck pain
- Pain radiating through an arm and/or leg
- Prominent lumps on the hands, feet or spine
- Numbness
- Burning
- Muscle cramps
Diagnosis 
Outlined below are some of the diagnostic tools that your physician may use to gain insight into your condition and determine the best treatment plan for your condition.
- Medical history: Conducting a detailed medical history helps the doctor better understand the possible causes of your back and neck pain which can help outline the most appropriate treatment.
- Physical exam: During the physical exam, your physician will try to pinpoint the source of pain. Simple tests for flexibility and muscle strength may also be conducted.
- X-rays are usually the first step in diagnostic testing methods. X-rays show bones and the space between bones. They are of limited value, however, since they do not show muscles and ligaments.
- MRI (magnetic resonance imaging) uses a magnetic field and radio waves to generate highly detailed pictures of the inside of your body. Since X-rays only show bones, MRIs are needed to visualize soft tissues like discs in the spine. This type of imaging is very safe and usually pain-free.
- CT scan/myelogram: A CT scan is similar to an MRI in that it provides diagnostic information about the internal structures of the spine. A myelogram is used to diagnose a bulging disc, tumor, or changes in the bones surrounding the spinal cord or nerves. A local anesthetic is injected into the low back to numb the area. A lumbar puncture (spinal tap) is then performed. A dye is injected into the spinal canal to reveal where problems lie.
- Electrodiagnostics: Electrical testing of the nerves and spinal cord may be performed as part of a diagnostic workup. These tests, called electromyography (EMG) or somato sensory evoked potentials (SSEP), assist your doctor in understanding how your nerves or spinal cord are affected by your condition.
- Bone scan: Bone imaging is used to detect infection,
malignancy, fractures and arthritis in any part of the skeleton.
Bone scans are also used for finding lesions for biopsy or excision.

- Discography is used to determine the internal structure of a disc. It is performed by using a local anesthetic and injecting a dye into the disc under X-ray guidance. An X-ray and CT scan are performed to view the disc composition to determine if its structure is normal or abnormal. In addition to the disc appearance, your doctor will note any pain associated with this injection. The benefit of a discogram is that it enables the physician to confirm the disc level that is causing your pain. This ensures that surgery will be more successful and reduces the risk of operating on the wrong disc.
- Injections: Pain-relieving injections can relieve back pain and give the physician important information about your problem, as well as provide a bridge therapy.
Treatment
The goal when treating bone spurs is to minimize pain and prevent any
additional joint damage. Treatment methods may include weight loss,
stretching and physical therapy, rest and ice. Injections can reduce
inflammation long enough to relieve symptoms. Medications such as
ibuprofen or injections may be administered for pain. Bone spurs
can be surgically removed in the case of serious damage and deformity.
[Top]
FAQs
How can osteoporosis impact the spine and cause a bone spur?
Osteoporosis can have extremely serious consequences on the spine. It is a degenerative condition in which joint cartilage can begin to wear down, causing bone to rub against bone. As a result, the body may begin to produce new bone to protect against this, which is how a bone spur forms.
 How can I tell if I have a bone
spur?
How can I tell if I have a bone
spur?
Bone spurs can generally be detected through X-ray, which can provide a visual of any bony deposits.
Do I need surgery to treat a bone spur?
Because bone spurs are usually evidence of an underlying problem, this
main problem should be addressed first. This can include treatment
methods for degenerative disc disease, arthritis and osteoporosis.
These conditions can often be successfully treated with nonsurgical
methods, such as interventional pain management.
[Top]