- Locations
- Find a Physician
- By Physician
- By Department
- The Center for Spine Health
- Hand & Wrist Center
- Shoulder & Elbow Center
- Foot & Ankle Center
- Joint Replacement Center
- The Sports Medicine Center
- Pediatric Orthopedic Center
- Trauma & Fracture Center
- Osteoporosis and Bone Health
- Oncology Center
- Cartilage Repair Center
- Concussion Rehab Center
- OrthoDirect
- Careers
- Patient Portal
- Intranet
 Degenerative Disc
Degenerative Disc
Overview | Causes | Symptoms | Diagnosis | Treatment | FAQ
Overview
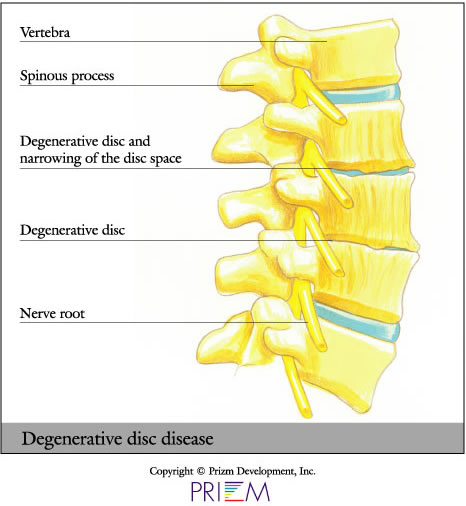
Degenerative disc disease frequently occurs with age. Discs become more brittle, less resilient and more prone to herniation. In many cases, the space between vertebrae can shrink and compress, which in turn can impinge upon nearby nerve roots, causing pain.
Degenerative disc disease is the single most common diagnosis related to serious back and neck pain. When a disc herniates in the spine, the surgeon can sometimes simply remove a portion of the disc. In other cases, where the disc is more damaged and must be removed, something must be placed into the disc space. Otherwise, the two vertebrae will collapse on top of one another, placing pressure on the nerve roots that branch off from the spinal cord.
Causes
Some of the contributing factors of degenerative disc disease are family history, lifestyle and age. The prime age for disc-related problems is after 35. If a parent had back or neck surgery for a herniated disc, you should be particularly concerned about taking care of your back. Lifestyle is another important factor. Those who perform frequent lifting or put themselves in situations where the spine is exposed to trauma or repetitive shock can also develop degenerative discs over time.
Osteoporosis can lead to disc degeneration bone fractures and pain symptoms. As bones become weaker, a person becomes increasingly at risk for vertebral fractures. Since osteoporosis typically doesn’t have noticeable symptoms, those at risk, particularly older women, should undergo a bone density scan in order to detect osteoporosis in its early stages. Dietary supplements or medications may be recommended to treat bone loss.
[Top]
Symptoms
Degenerative disc disease makes the back more prone to injury and can contribute to the following conditions:
- Back pain
- Neck pain
- Hunched over appearance
- Herniated disc
- Vertebral fractures
Diagnosis
Outlined below are some of the diagnostic tools that your physician may use to gain insight into your condition and determine the best treatment plan for your condition.
- Medical history: Conducting a detailed medical history helps the doctor better understand the possible causes of your back and neck pain which can help outline the most appropriate treatment.
- Physical exam: During the physical exam, your physician will try to pinpoint the source of pain. Simple tests for flexibility and muscle strength may also be conducted.
- X-rays are usually the first step in diagnostic
testing methods. X-rays show bones and the space between bones.
They are of limited value, however, since they do not show muscles
and ligaments.

- MRI (magnetic resonance imaging) uses a magnetic field and radio waves to generate highly detailed pictures of the inside of your body. Since X-rays only show bones, MRIs are needed to visualize soft tissues like discs in the spine. This type of imaging is very safe and usually pain-free.
- CT scan/myelogram: A CT scan is similar to an MRI in that it provides diagnostic information about the internal structures of the spine. A myelogram is used to diagnose a bulging disc, tumor, or changes in the bones surrounding the spinal cord or nerves. A local anesthetic is injected into the low back to numb the area. A lumbar puncture (spinal tap) is then performed. A dye is injected into the spinal canal to reveal where problems lie.
- Electrodiagnostics: Electrical testing of the nerves and spinal cord may be performed as part of a diagnostic workup. These tests, called electromyography (EMG) or somato sensory evoked potentials (SSEP), assist your doctor in understanding how your nerves or spinal cord are affected by your condition.
- Bone scan: Bone imaging is used to detect infection, malignancy, fractures and arthritis in any part of the skeleton. Bone scans are also used for finding lesions for biopsy or excision.
- Discography is used to determine the internal structure of a disc. It is performed by using a local anesthetic and injecting a dye into the disc under X-ray guidance. An X-ray and CT scan are performed to view the disc composition to determine if its structure is normal or abnormal. In addition to the disc appearance, your doctor will note any pain associated with this injection. The benefit of a discogram is that it enables the physician to confirm the disc level that is causing your pain. This ensures that surgery will be more successful and reduces the risk of operating on the wrong disc.
- Injections: Pain-relieving injections can relieve back pain and give the physician important information about your problem, as well as provide a bridge therapy.
 Treatment
Treatment
A typical solution for problems related to DDD is a spinal fusion procedure.The main problem with fusion surgeries is that they don't often turn out well. While some studies claim a success rate of about 75 percent, that still leaves one in four surgeries as not successful. The second problem with fusion surgery is that there is a reduction in mobility that can cause other problems over time. Because the fusion locks a vertebral segment from rotating, it causes more stress on the level above and below the fused site, which in turn can herniate the other discs. Thankfully, there is an alternative today - artificial disc implantation.
Dietary supplements or medications may be recommended
to treat degenerative disc disease that is linked to osteoporosis.
[Top]
FAQs
What is degenerative disc disease?
A natural byproduct of aging is the loss of resiliency in spinal discs and a greater tendency for them to herniate, especially when placed under a weighty load, like when we lift heavy objects. Additionally, some people have a family history of degenerative disc disease, which increases their own risk of developing it. When a natural disc herniates or becomes badly degenerated, it loses its shock-absorbing ability, which can narrow the space between vertebrae.
Who is a candidate for the artificial disc?
Patients with a diseased disc between L4 and L5 or between L5 and S1 (all in the lower back) that is worn out or become injured and causes back pain are candidates for the artificial disc. Other candidates include those with degenerative disc disease (DDD) whose bones (vertebrae) have moved less than 3mm. Your physician will help you determine whether or not the artificial disc is a good choice for you. Factors that will be considered include your activity level, weight, occupation and allergies.
-
What are the benefits of the artificial disc?
Generally speaking, those who receive artificial disc replacements return to activity sooner than traditional fusion patients. Also, because there is no need to harvest bone from the patient’s hip, there is no discomfort or recovery associated with a second incision site. Some of the overall benefits of artificial disc surgery include:
- Retains movement and stability of the spine
- Prevents degeneration of surrounding segments
- No bone graft required
- Quicker recovery and return to work
- Less invasive and painful than a fusion
- Reduces pain associated with disc disease
While the artificial disc may well be a promising new technology, most spine surgeons today are very cautious. There are many serious concerns including:
- Constantly changing technology as new discs are coming out that last longer and may be easier to insert and remove
- The lifespan of the implants are in question
- What happens if the implant needs to be removed
Consult with your spine surgeon to determine your best
option.
[Top]