- Locations
- Find a Physician
- By Physician
- By Department
- The Center for Spine Health
- Hand & Wrist Center
- Shoulder & Elbow Center
- Foot & Ankle Center
- Joint Replacement Center
- The Sports Medicine Center
- Pediatric Orthopedic Center
- Trauma & Fracture Center
- Osteoporosis and Bone Health
- Oncology Center
- Cartilage Repair Center
- Concussion Rehab Center
- OrthoDirect
- Careers
- Patient Portal
- Intranet

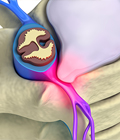
About the Artificial Disc
Perhaps the most anticipated advance in spine surgery over the past 20 years was the creation of the first artificial disc. The first artificial disc in the United States received formal approval by the Food and Drug Administration (FDA) for widespread use in the United States on October 26, 2004. While this technology is somewhat new to the U.S., the first artificial disc was implanted in Europe in 1959 with others following in the 1970s. So artificial disc technology has been evolving over the last 50 years so the concept is far from new.
In fact, the artificial disc for the spine is simply the same concept as replacing a worn out hip joint, knee joint or shoulder joint. In the early 1900s patients had these joints fused which was an awful outcome. Thankfully joint replacements have been in use for more than 70 years and are now done in outpatient surgery with the person going home the same day. Unlike knee and hip replacement patients who are typically in their 50s or 60s, many spine patients can benefit from artificial disc technology at a much younger age — in their 20s or 30s. The implantation of an artificial disc in younger patients can raise a surgeon’s concern about the potential life span of the artificial disc in the spine and the need for revision surgery to replace a worn-out artificial disc, which can be complex.
 For example, it’s estimated that more than 1 million people have neck problems caused by disc herniations. Each year in the U.S. there are about 300,000 neck surgeries. It is estimated that now half of neck surgeries performed now use an artificial disc.
For example, it’s estimated that more than 1 million people have neck problems caused by disc herniations. Each year in the U.S. there are about 300,000 neck surgeries. It is estimated that now half of neck surgeries performed now use an artificial disc.
One of the main drivers for the use of artificial discs was new research a few years ago from the North American Spine Society (the largest group of international spine surgeons) that documented that artificial disc replacement in the cervical spine is now the preferred alternative to spinal fusion. The research found that the artificial disc reduces adjacent segment disease and lessens the risk of future disc herniations at other levels in the neck.
With that said, it is important to remember that this technology is still evolving with new implants continually in development. In addition, other artificial disc models are available on a limited basis through “clinical trials” where a patient agrees to be part of clinical study designed to measure the success of a new disc model, which will be part of an FDA study. Patients who participate in a clinical trial can gain access to the most current technology, even though it has yet to gain FDA approval for use in the U.S.
An Alternative to Fusion Surgery
 The artificial disc concept is intended to be an alternative for spinal fusion surgery. During a fusion procedure, the damaged disc is typically replaced with bone from a patient’s hip or from a bone bank. Fusion surgery causes two vertebrae to become locked in place, putting additional stress on discs above and below the fusion site, which restricts movement and can lead to further disc herniation with the discs above and below the degenerated disc.
The artificial disc concept is intended to be an alternative for spinal fusion surgery. During a fusion procedure, the damaged disc is typically replaced with bone from a patient’s hip or from a bone bank. Fusion surgery causes two vertebrae to become locked in place, putting additional stress on discs above and below the fusion site, which restricts movement and can lead to further disc herniation with the discs above and below the degenerated disc.
When a natural disc herniates or becomes badly degenerated, it loses its shock-absorbing ability, which can narrow the space between vertebrae. In fusion surgery, the damaged disc isn’t repaired but rather is removed and replaced with bone that restores the space between the vertebrae. However, this bone locks the vertebrae into place, which can then damage other discs above and below. An artificial disc replacement is intended to duplicate the function level of a normal, healthy disc and retain motion in the spine.
A common aspect of all artificial discs is that they are designed to retain the natural movement in the spine by duplicating the rotational function of the discs. Most artificial disc designs have plates that attach to the vertebrae and a rotational component that fits between these fixation plates. These components are typically designed to withstand stress and rotational forces over long periods of time. Still, like any manmade material, they can be affected by wear and tear.
Which artificial disc is best?
Currently, more than 10 artificial discs have secured FDA approval for use in the United States and the number is growing each year.
For many spine surgeons, the rapidly changing array of artificial discs that are being innovated represents a tough decision for WHICH disc to recommend to patients. For example, newer discs making it through the rigorous FDA approval process are now starting to provide up-and-down shock absorption in addition to rotation. This is especially important for low back discs that must support the weight of the trunk.
Other elements in the latest technology artificial discs are surfaces that may last years longer, which would eliminate a revision surgery because the disc outlives the patient. This is the same dilemma faced by total joint surgeons who for years tried to delay a hip or knee replacement until a person reaches their fifties or sixties with the strategy that the joint will outlive the patient and eliminate the need for a complex revision surgery. In particular, with knee or hip replacement, the surgeon has much easier access to the joint during revision surgery, rather than having to work through the abdomen to access the front of the spine and remove a worn out disc.
The conundrum with delaying joint replacement surgery, or artificial disc surgery, is that patients want mobility while they are young enough to enjoy it.
University Orthopedics spine surgeons are trained in several of the FDA approved artificial discs. The two most commonly used artificial discs are the M6 artificial disc and the Mobi-C artificial disc.
The M6 Artificial Disc
 The M6 disc was FDA approved in 2019. The disc mimics the shock absorption of a natural disc by using an artificial visco-elastic nucleus and fiber annulus in its design. This unique design allows for shock absorption at the implanted level as well as retains a range of motion. The polyurethane center makes the disc compressible — to imitate the function of the natural disc — and able to absorb shock.
The M6 disc was FDA approved in 2019. The disc mimics the shock absorption of a natural disc by using an artificial visco-elastic nucleus and fiber annulus in its design. This unique design allows for shock absorption at the implanted level as well as retains a range of motion. The polyurethane center makes the disc compressible — to imitate the function of the natural disc — and able to absorb shock.
By comparison, most traditional artificial discs have polyethylene cores which glide back and forth to accommodate motion, but they aren’t compressible. Aside from the compressibility of the disc, the M6 functions like other artificial discs to alleviate the pain associated with a herniated disc and enable patients to preserve the natural motion. This is especially crucial with the neck which has only 7 cervical vertebrae to provide motion. While there are limited clinical studies that document the superior capabilities of the M6 disc over other options, the M6 disc is one of the most favored discs used by spine surgeons in Europe for total disc replacement.
 The Mobi-C Artificial Disc
The Mobi-C Artificial Disc
The Mobi-C is one of the most widely used cervical discs in the world. Mobi-C has been in use since 2004 (about 20 years ago) and has since been implanted in more than 17,000 spinal levels in 25 countries. Mobi-C is different in that it limits damage to the bone as the surgeon is able to install without chisel cuts into the small vertebral bodies of the cervical spine.
The Mobi-C has a polyethylene core to slide and rotate inside the disc to preserve motion in the cervical spine. It also is designed to reduce the stress between the implant and adjacent bone which eliminates invasive fixation devices used by other discs.
The Mobi-C disc gained a lot of attention as the first FDA approved disc for use at TWO levels in the neck. This was an important capability as some patients with degenerative disc disease had herniations at multiple levels in the back. Using fusion to treat those herniations would lock the neck and prevent any motion. The Mobi-C disc also provides bone sparing fixation without chisel cuts into the small vertebral bodies of the cervical spine.
If it important to remember that the spine surgeon considers MANY issues in selecting a disc for a patient. This includes the patient's disc issue and which artificial disc is a better fit. Some discs, for example, come in different sizes recognizing the difference between a petite woman and a tall man.
Benefits
Some of the main benefits of the artificial disc parallel that of knee replacement and hip replacement. This can include the following benefits:
- An artificial disc in the neck or back retains motion in that particular segment of the spine.
- It prevents degeneration of disc levels above and below the affected disc
- There is no bone graft required
- There can be a quicker recovery and return to work or activity
- It can be a less invasive and less painful surgery than a fusion
- There can be less blood loss during surgery
Lumbar vs. Cervical Artificial Discs
 Because of the weight of the body and the rotational stress that the trunk places on discs in the low back (lumbar) area, more stress is placed on artificial discs in the lumbar area than in the neck (cervical) area, which only supports the weight of the head.
Because of the weight of the body and the rotational stress that the trunk places on discs in the low back (lumbar) area, more stress is placed on artificial discs in the lumbar area than in the neck (cervical) area, which only supports the weight of the head.
A second issue relates to the ease of the artificial disc surgery and any necessary revision surgery to replace a worn out artificial disc. Because the surgeon must access the front of the spine, an incision is made in the abdomen for lumbar discs and in the front of the neck for cervical discs. Access to the cervical discs can be easier than the lumbar discs.
Consequently, most spine surgeons favor artificial discs in the neck because the neck is easier to access than the lumbar spine, and revision surgery is less complex. Also artificial discs for the low back are evolving rapidly with some designs accessing the spine from the back rather than the complex surgery through the stomach to reach the front of the spine.
Other issues to consider
When treating knee and hip replacement patients, orthopedic surgeons try to postpone the implantation of an artificial joint until a patient is at least 50 years old so that they do not outlive their artificial joint, which typically lasts anywhere from 15 to 20 years. Revision surgery, which may be necessary to replace a worn-out artificial joint, can be complex.
This is also a concern with the artificial disc. Unlike knee and hip replacement patients who are typically in their 50s or 60s, many patients can benefit from artificial disc technology at a much younger age — in their 20s or 30s. Therefore, the implantation of an artificial disc in younger patients can raise a surgeon’s concern about the potential life span of the artificial disc in the spine and the need for revision surgery to replace a worn-out artificial disc, which can be complex.
In summary, some spine surgeons may be cautious about the use of artificial discs for the following reasons:
- Wear and tear on an artificial disc can require revision surgery in 10 to 20 years that can be complex.
- Most artificial disc implants only address rotational forces, not the up and down shock absorbing function of the natural disc.
- Overweight and obese people can wear out a lumbar disc prematurely.
- New artificial discs are continually in development.
- There are not many 20-year-long studies that show the long-term effects of wear and tear on artificial disc implants in the low back.

Frequently Asked Questions about the Artificial Disc
Q. My other spine surgeon suggested an Anterior Cervical Discectomy and Fusion (ACDF) for my neck. Why is spinal fusion in the neck a problem?
A. With only 6 discs in the neck, fusing one level leaves only 5 disc levels for your neck to have rotation. Research from the North American Spine Society has documented that when you fuse one level, it can cause herniations at the other levels. So a person who has an ACDF could need another neck surgery for other disc levels, which then prevents any normal rotation. Driving a car and being unable to turn your head would be difficult, as would playing golf, tennis, or pickle ball.
Q. Is reversal of spinal fusion possible?
A. Not really. While there are some spine surgeons providing this, reversal of a spinal fusion is a complex spine surgery and may cause new pain symptoms because the bone graft becomes fused to the facet joints at the back of the spine. Cutting out that bone graft then causes a new pain from the disrupted fact joints. That’s why it’s best to explore an artificial disc as the first surgery.
Q. My surgeon says I am not a candidate for an artificial disc. Why not?
A. Not everybody qualifies to have their herniated disc replaced with an artificial implant. If your surgeon is proficient in artificial disc surgery and does a high volume of it, he or she probably has determined correctly that you would not have a good outcome from an implant.
Q; Why are there so many different artificial disc models used?
A. When the first artificial discs were introduced, they were all the same size — about the size of a quarter. Now artificial discs come in different sizes and and designs to create a better fit for a woman vs. a large man as the vertebrae in those two people are significantly different. Other changes related to the disc design and how that helps installation. Some have a keel that firmly locks into place and fixates between the vertebrae. All these factors are considered by the trained spine surgeon.
Q; Why is my health insurance company resistant to paying for an artificial disc?
A. Some health insurance companies are slow to embrace new technology even after it has become mainstream. Some may be hesitant because they are afraid that a bad outcome could result in a lawsuit. Others do not like paying for new technology which may be more expensive than an older procedure — albeit with a worse outcome for the patient. Thankfully, more mainstream health insurance companies are covering artificial disc replacement for the neck as they learn an artificial disc can prevent a second surgery for another disc level.