- Locations
- Find a Physician
- By Physician
- By Department
- The Center for Spine Health
- Hand & Wrist Center
- Shoulder & Elbow Center
- Foot & Ankle Center
- Joint Replacement Center
- The Sports Medicine Center
- Pediatric Orthopedic Center
- Trauma & Fracture Center
- Osteoporosis and Bone Health
- Oncology Center
- Cartilage Repair Center
- Concussion Rehab Center
- OrthoDirect
- Careers
- Patient Portal
- Intranet
![]() Overview | Causes | Symptoms | Diagnosis | Treatment | FAQ
Overview | Causes | Symptoms | Diagnosis | Treatment | FAQ
Overview
The spine is composed of many vertebrae stacked on top of each other. Between these bones are discs, which act as shock absorbers. The shock absorbing discs resemble jelly donuts, each having a jelly-like center. As we age, the discs naturally become less flexible and more brittle.
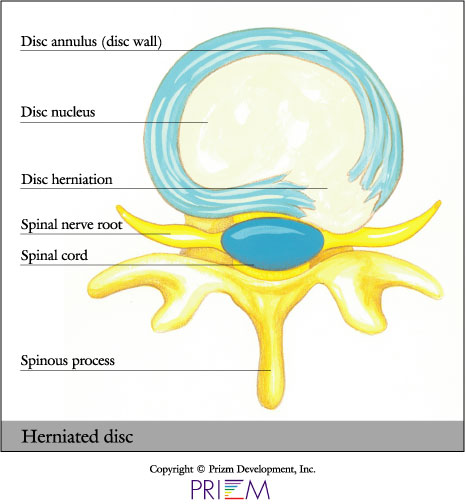
In the event of a fall or heavy strain, these discs can rupture, causing the nucleus to break through the wall of the disc and place pressure on the nerves that branch out from the spinal cord. This results in a herniated disc, accompanied by back or neck pain.
As the nucleus escapes through the wall, the tissue either remains connected with the disc, or it can break from the nucleus and travel away from the disc. Discs can herniate in any direction — forward, centrally, or most commonly, backwards and sideways in the direction of the spinal nerves.
Sometimes, people mistake excruciating pain for a herniated disc, when the pain might actually be the signal of a muscle strain. The most common indicator of a herniated disc is when pain radiates down into the leg or arm.
Special extension exercises can help relieve pain from a herniated disc. Exercise can work like a vacuum to suck the center of the disc back into place, helping release pressure on the nerve. Although someone suffering an attack of back pain may find it hard to believe, it has been proven that specific exercises can help relieve some cases of back or neck pain.
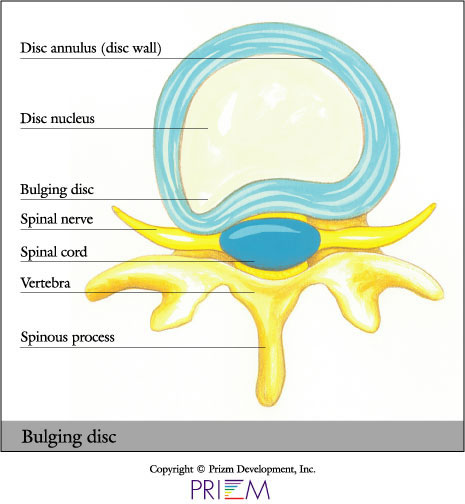
While herniated discs are often referred to as “slipped discs,” this really isn’t accurate because discs don’t ever slip out of position. They are actually attached by connective tissue to vertebrae above and below. A disc herniation can be “contained” or “uncontained.” With a bulge, for example, the jelly center remains within the disc wall. "Uncontained" means the jelly center has broken through the annulus wall but stays connected to the nucleus pulposus. Or the herniation can be “sequestered,” when it breaks free from the nucleus and travels away from the disc.
The good news is that a herniated disc does not necessarily mean a person needs surgery. In some cases, symptoms from a minor herniation can subside, and with care, pain recurrences can be minimized.
A bulging disc forms when the wall of the disc is deformed but not necessarily herniated. The nucleus is still contained in the wall. You don't need surgery to treat a bulging disc.
[Top]
Causes
In the event of a fall or heavy strain, discs can rupture, causing
the nucleus to break through the wall of the disc and place pressure
on the nerves that branch out from the spinal cord. This results
in a herniated disc, accompanied by back or neck pain. For example,
sitting down for a while, then lifting a heavy object, can cause
a disc to herniate.
[Top]
Symptoms
Sometimes, people mistake excruciating pain for a herniated disc, when the pain might actually be the signal of a muscle strain.
Because the nerve roots act as telegraph lines to other
parts of the body, a common complication of disc herniation is that
it can cause pain that is felt in other parts of the body. In fact,
leg pain below the knee is a common herniated disc symptom. This radiating
pain is called radicular pain or radiculopathy. Often, back pain without
leg pain can be a result of partial herniation of the disc or an internal
disc disruption.
[Top]
Diagnosis
Outlined below are some of the diagnostic tools that your physician may use to gain insight into your condition and determine the best treatment plan for your condition.
- Medical history: Conducting a detailed medical history helps the doctor better understand the possible causes of your back and neck pain which can help outline the most appropriate treatment
- Physical exam: During the physical exam, your physician will try to pinpoint the source of pain. Simple tests for flexibility and muscle strength may also be conducted.
- X-rays are usually the first step in diagnostic testing
methods. X-rays show bones and the space between bones. They are
of limited value, however, since they do not show muscles and ligaments.

- MRI (magnetic resonance imaging) uses a magnetic field and radio waves to generate highly detailed pictures of the inside of your body. Since X-rays only show bones, MRIs are needed to visualize soft tissues like discs in the spine. This type of imaging is very safe and usually pain-free.
- CT scan/myelogram: A CT scan is similar to an MRI in that it provides diagnostic information about the internal structures of the spine. A myelogram is used to diagnose a bulging disc, tumor, or changes in the bones surrounding the spinal cord or nerves. A local anesthetic is injected into the low back to numb the area. A lumbar puncture (spinal tap) is then performed. A dye is injected into the spinal canal to reveal where problems lie.
- Electrodiagnostics: Electrical testing of the nerves and spinal cord may be performed as part of a diagnostic workup. These tests, called electromyography (EMG) or somato sensory evoked potentials (SSEP), assist your doctor in understanding how your nerves or spinal cord are affected by your condition.
- Bone scan: Bone imaging is used to detect infection, malignancy, fractures and arthritis in any part of the skeleton. Bone scans are also used for finding lesions for biopsy or excision.
- Discography is used to determine the internal structure of a disc. It is performed by using a local anesthetic and injecting a dye into the disc under X-ray guidance. An X-ray and CT scan are performed to view the disc composition to determine if its structure is normal or abnormal. In addition to the disc appearance, your doctor will note any pain associated with this injection. The benefit of a discogram is that it enables the physician to confirm the disc level that is causing your pain. This ensures that surgery will be more successful and reduces the risk of operating on the wrong disc.
- Injections: Pain-relieving injections can relieve back pain and give the physician important information about your problem, as well as provide a bridge therapy.
Treatment
Unlike muscles, which can heal somewhat quickly, a torn or degenerated disc heals more slowly. The good news is that in many cases, the pain and inflammation originating from damaged discs can be treated nonsurgically by reducing the inflammation and by strengthening the musculature surrounding the damaged disc to give it more support.
Special extension exercises can help relieve pain from
a herniated disc. Exercise can work like a vacuum to suck the center
of the disc back into place, helping release pressure on the nerve.
Although someone suffering an attack of back pain may find it hard
to believe, it has been proven that specific exercises can help relieve
their pain.
[Top]
FAQs
What caused my disc to herniate?
Herniated discs can occur as a result of a heavy strain or fall, which
causes the nucleus to break through the wall of the disc and place
pressure on the nerves that branch out from the spinal cord. For example,
lifting a heavy object after sitting down for a long period of  time
can cause a disc to herniate.
time
can cause a disc to herniate.
What is the best way to treat a herniated disc?
Nonsurgical treatment methods are always the best option to try first.
This will most likely involve working with a physical therapist who
will develop a customized exercise program involving specific stretches
and extension movements for you.
[Top]