- Locations
- Find a Physician
- By Physician
- By Department
- The Center for Spine Health
- Hand & Wrist Center
- Shoulder & Elbow Center
- Foot & Ankle Center
- Joint Replacement Center
- The Sports Medicine Center
- Pediatric Orthopedic Center
- Trauma & Fracture Center
- Osteoporosis and Bone Health
- Oncology Center
- Cartilage Repair Center
- Concussion Rehab Center
- OrthoDirect
- Careers
- Patient Portal
- Intranet
Causes of knee pain | Understanding symptoms | Diagnostics | Nonsurgical treatments | Surgical options | Joint Replacement | Knee prevention
Knee pain? You’re not alone.
If you have knee pain, rest assured you are far from alone. Each year 6 million Americans head to the doctor for knee pain issues. This translates into 2.5 percent of the U.S. population sitting in doctors’ offices for relief of knee pain. Even more people try to self-diagnose and treat themselves with pain pills, anti-inflammatories and home remedies.
A U.S. study found that 18% of men aged 60 years and older reported knee pain, and that percent goes up as we age. Women experience knee pain even more than men.
But it’s important to remember that pain symptoms are typically a warning mechanism to our brains that something is wrong that needs to be addressed. Simply masking pain symptoms with drugs, or even just anti-inflammatories, can have long term impact on internal organs and one’s lifespan. Masking symptoms can also encourage the person to further overuse and injure their knee joint.
Consequently, it’s important to address knee pain symptoms early on to determine if there are non-surgical or surgical treatment options that can relieve pain symptoms without drugs or pills.
Step #1 is understanding the complex knee joint and how it works so you can better relate to treatment options that may be recommended by a knee specialist.
What causes knee pain?
Any mechanical device can and will fail if placed under excessive strain. That could be a fall down stairs or banging the knee into a dashboard during a car accident. But again, accidents and falls represent a relatively small percent of knee pain cases.
The vast majority of knee pain issues develop over a period of years. In these cases, the knee becomes like a creaky or unstable hinge that doesn’t get better, either because components in the knee are weak or unstable, or the lubrication in the joint and bone surface have been eroded over time.
That’s the bad news. The good news is that of all knees that hobble into doctors’ offices every year, only 20 percent will need surgery. Of those that don’t need surgery, many can get better with time and new non-surgical treatment options.
In some cases anti-inflammatories and specialized exercises increase range of motion, flexibility, strength, and resistance to future knee strain are usually prescribed. Sometimes knee braces are also used.
Knee anatomy
The knee is a complex mechanism which absorbs shock as we jump, and is extremely flexible, permitting a change in direction while running at high speeds. The knee joint is composed of ligaments, which provide support, and muscles for strength.
The healthy young knee joint is a lubricated mechanism, which functions reliably unless twisted, bruised or broken. For example, of all the areas treated by orthopedic surgeons, the knee is the most commonly injured joint, representing 26 percent of orthopedic visits, followed by the spine (17 percent) and hip (15 percent).
Some cases of knee pain are caused by trauma, such as a fall or a car crash. According to the American Academy of Orthopedic Surgeons (AAOS), over a lifetime, each American will suffer two fractures. Many of which will occur at the knee.
However, trauma or fracture represents a small percentage of knee problems. The majority result from repetitive wear and tear. In these cases, the cartilage or joint surfaces are slowly damaged over time. One type of chronic injury is arthritis, which might be thought of as a “rusting” of the knee joint. It causes pain and robs the knee of flexibility. Indeed, half of all knee pain may be tied in some way to arthritis.
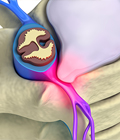
Cartilage is a natural lubricant tissue that helps your joints move smoothly. When cartilage begins to break down with age or injury, you experience bone-on-bone friction which causes symptoms like inflammation, knee pain, stiffness or inability to move the joint without extreme pain.
Many of the causes of osteoarthritis are out of a person’s control, e.g. heredity or accidental injury. But you can make lifestyle changes to reduce your risk of arthritis, ligament strain and a painful knee.
What things could cause knee pain?
Tendons are cords of strong, fibrous tissue, which connect muscle to bone. Muscle power is transferred across tendons to bones. The primary muscle groups associated with the knee are the quadriceps and hamstring muscles. These muscles are at work when the knee is extended, flexed, or rotated.
The easiest way to understand how the muscles in the leg operate is to imagine two large rubber bands, one that runs down the front, and another that runs down the back. The front rubber band pulls the leg straight, or extends it. The rear rubber band causes the leg to do the reverse, or flexes it.
The quadriceps mechanism is the strongest muscle in the leg, allowing us to walk and run. The quadriceps mechanism includes:
- Quadriceps muscle
- Quadriceps tendon above the patella
- Patella
- Patellar tendon
The quadriceps tendon connects the quadriceps muscle to the patella, while the patellar tendon connects the patella to the tibia. The hamstring muscles at the back of the thigh, as well as the calf muscles, enable the knee to flex.
Working together, the muscles, tendons, and ligaments of the knee work fluidly. Turn to any sports channel on a Sunday afternoon and pay attention to the slow motion videos of a wide receiver running a complex pass route, jumping through the air to snatch a football, and then changing directions and accelerating into the end zone. Or watch a skier charge through a slalom course, knees pumping as they work the edges of their skis through the gates.
That’s when everything is working perfectly. Things change after a wide receiver takes a blow to the side of the knee, or when that downhill skier catches an edge and tumbles.
The Most Common Knee Problems
Knee pain can start with issues from overuse or strain. Most knee problems come from the following areas:
Pain from the kneecap. Those with kneecap pain typically notice an increase in pain when going up or down stairs, when running downhill, or even while sitting.
 Torn meniscus. The bottom of the femur (thigh bone) and the top of the tibia (shin bone) that come together in the knee joint, are covered by cartilage which enables the bones to glide against each other with a minimal amount of friction. But if the knee is twisted, or banged, the cartilage can become damaged or loosened out of its normal position. A common symptom of this type of injury is that the knee may “catch” or grind at a certain point as it moves through its normal range of motion.
Torn meniscus. The bottom of the femur (thigh bone) and the top of the tibia (shin bone) that come together in the knee joint, are covered by cartilage which enables the bones to glide against each other with a minimal amount of friction. But if the knee is twisted, or banged, the cartilage can become damaged or loosened out of its normal position. A common symptom of this type of injury is that the knee may “catch” or grind at a certain point as it moves through its normal range of motion.
Ligament problems. If you think of the knee as a hinge between the upper leg and lower leg, it is the awesome work of the supporting muscles, ligaments, and tendons to make sure that it is supported and working properly—often while the leg is twisting, turning and absorbing shock from jumping. There are four key ligaments that can be injured in the knee:
Anterior cruciate ligament (ACL) is often the victim of non-contact injury, where the knee is twisted while the foot is planted. You may feel a pop, and the whole knee may give way.
Posterior cruciate ligament (PCL) injuries can be caused by a blow to the knee, or when the knee is forced backward.
Medial collateral ligament (MCL) can be injured from a blow to the outside area of the knee.
Lateral collateral ligament (LCL) injury can be caused by a blow to the inside area of the knee.
Tendon problems. Sometimes the tendons that attach the kneecap (patella) to the shinbone (tibia) can become inflamed.
Arthritis. Aside from pain from ligament and tendon problems, osteoarthritis accounts for a large percent of knee pain symptoms and is the most difficult to treat. The incidence of an arthritic joint goes up with age.
Osgood-Schlatter disorder. This is an overuse problem where the quadriceps tendon causes inflammation in the knee. This disorder is more common in children and teens.
Why are ligaments so easily damaged?
 Consider the average size of the ACL or PCL. They’re smaller than you might think. The ACL is about one centimeter wide and has a range of eight to thirteen millimeters wide, while the PCL is thirteen to sixteen millimeters. Both of these ligaments are only about four centimeters in length.
Consider the average size of the ACL or PCL. They’re smaller than you might think. The ACL is about one centimeter wide and has a range of eight to thirteen millimeters wide, while the PCL is thirteen to sixteen millimeters. Both of these ligaments are only about four centimeters in length.
The sound of an ACL as it tears is distinctive, and the feeling unforgettable. Here’s what happens. The anterior cruciate ligament tightens as the knee is twisted. But when the knee is forced past the normal straightened position, or when the tibia is twisted excessively outward on the femur, or frequently when the knee is struck from the side, the ACL may be stretched beyond its breaking point. Those nearby will notice a distinctive popping sound, and the afflicted individual will experience a sudden burst of pain and instability. Often the knee buckles, causing a fall to the floor. Swelling appears promptly. Swelling and pain may subside, but after returning to sports, there will be a sense of instability with any twisting maneuver. While not commonly the case, bleeding may occur in the knee. Because the knee is now rendered unstable, repeated injury can now damage the menisci or articular cartilage and ultimately lead to arthritis. Now that you have an understanding of the gears and moving parts that make up the knee joint, we start to understand what can go wrong.
Knee - Strains, Sprains, and Tears
Strains are common and occur when a muscle is overworked or overstretched. When you suddenly dive into a new activity or exercise program, you often strain a muscle or tendon by overworking it. A strained muscle is what we sometimes call a “pulled” muscle. A strain is characterized by a sharp pain or “stitch” at the time of injury. The area becomes sore and stiff within a few hours or moments of straining. Pain accompanies further movement but often subsides within days. Strains often occur when, after months of inactivity, we throw ourselves into a new exercise routine. If you are out of shape and haven’t carefully stretched your muscles, think twice before zealously jumping on the treadmill and powering it up to a high-speed performance level. When the machine starts racing, your legs might race right out from under you, and in that case, you’ll be lucky if a strain is the only injury suffered. Sprains are more serious than strains. A sprain occurs when a ligament is overstretched or partially torn. Since ligaments hold bones together, their close proximity to the bone may lead to the suspicion of a fracture. The signs of a sprain include joint pain, inflammation, tenderness and swelling. These may be associated with black and blue discoloration. Sprains in the knee involve partial tears to the ACL, PCL, MCL, and LCL. The location of the injury should clarify any confusion over whether it’s a sprain or strain. Strains occur in the muscles of the neck, back, thighs, and calves. Sprains are found around joints—knees, ankles, or wrists. Tears are more severe than strains or sprains. When muscles, ligaments, or tendons are torn they are actually disrupted. The torn ends grossly disrupt the continuity of their structure.
Ligament tears:
Picture a tall radio tower, that has four main cables that anchor it to the ground. You knee is similar. It has four main “ligaments” that hold it in place: ACL, PCL, MCL, and LCL. Unless you are a football player who is tackled roughly around the knees, which can tear any of these four, 90% of the time the ACL — anterior cruciate ligament — is the single ligament that most often tears. It’s the one that weaves from the front of the shin, through the kneecap, and attaches to the thighbone.
If you are playing tennis, for example, and you stretch to reach a ball, and hear a pop, chances are you tore your ACL. The sensation is then followed by a feeling of instability, wobbliness and pain, and sometimes nausea. You typically have no doubt that something terrible has gone wrong and you stop playing. You officially have had a bad day.
If the ACL is partially torn, non-surgical treatment, customized therapy and rest can in some cases heal the tear.
A complete tear however needs surgery to repair it. During surgery, the knee surgeon harvests a tendon from either your hamstring or your patellar tendon, and weaves a new ACL into place and anchors it on the femur and tibia. The good news is that ACL surgery is somewhat common and done in day surgery. With some rehab, and some customized exercises, you’ll be back in action within a couple months.
Pain from ACL Tears
The anterior cruciate ligament (ACL) is deep within the knee. It crisscrosses the posterior cruciate ligament (PCL) and keeps the tibia from sliding too far forward in relation to the femur. The PCL does the opposite. It prevents the tibia from sliding excessively backwards. The PCL is further supported by two minor ligaments: the ligaments of Humphry and Wrisberg. The ligaments that provide sidewise stability to the knee are the medial collateral ligament (MCL) and lateral collateral ligament (LCL). These ligaments limit side-to-side motion.
When the ACL is torn, it is often because the leg rotates while the foot stays planted on the ground. Often times an ACL tear is accompanied by a loud popping sound from the knee and the support of the knee gives way. A posterior cruciate injury happens when the knee is forced backwards or when it receives a hard impact. A medial collateral ligament injury most commonly occurs when the knee is hit from the outside while a lateral collateral ligament injury occurs when the knee is impacted from the inside.
Pain from Meniscus Tears
To keep the top of the shin (tibia) from rubbing on the bottom of the thighbone (femur), Mother Nature provided us meniscus tissue that acts as a shock absorber pad and lubricant between the bones. But abuse and excessive wear and tear can tear this protective tissue. That again can require a minimally invasive surgery to correct.
Meniscal tears can occur at any age. In the younger age group, they are usually sports-related and result from violent trauma. Contact sports like football account for a large number of tears. The type of movement that most often causes meniscal injury is one in which the foot is firmly planted on the ground while the knee is twisted. Shoes with cleats often contribute to this type of injury by anchoring the lower leg into the ground and preventing it from moving with the knee.
Along with other sports, which call for cutting, pivoting, or decelerating, basketball and tennis can also lead to meniscal tears. Traumatic meniscal injuries may also be accompanied by the tearing of a ligament, such as the anterior cruciate ligament.
For those forty and older, meniscal tears are less likely to be due to sports injury. With age the meniscus weakens and becomes more fragile. Individuals in this age group can tear a meniscus by performing simple activities, such as squatting.
Meniscal tears come in a variety of sizes and shapes. Often torn fragments lodge between the tibia and femur causing mechanical obstruction and pain. When this happens, the knee is said to “lock up” which means that the patient is unable to extend the knee fully outward. Fluid accumulates as the result of an inflammatory process, and walking becomes difficult.
Menisci lack blood supply except at their outer rim. Once torn, they heal poorly, if at all, and function is lost. Symptoms often vary in intensity depending upon the level of one’s activity.
Fractures
A bone can break for a number of reasons. A traumatic injury such as a car accident can cause a bone to break. Other causes for bones breaking can be "stress" fractures where a bone is used repetitively and because of compression, it breaks.
Dislocation
Sometimes, especially while doing something physically strenuous, we can throw a joint out of alignment with the bone. Although nothing breaks, the alignment is off. This is called dislocation.
Chondromalacia
“Chondro” indicates cartilage, while “malacia” means softening. Consequently, chondromalacia together means softening of the cartilage. But chondromalacia really refers specifically to softening of the under surface of the patella, or kneecap. It is a degenerative condition which occurs as the result of chronic wear of the kneecap against the femur. The articular cartilage gradually softens and then frays.
At other times, a traumatic blow around the knee is the cause of chondromalacia. Symptoms of chondromalacia include pain in front of the knee, especially when walking up and downhill, stiffness after prolonged sitting, and a grinding or clicking sensation as the knee is flexed and extended.
Symptoms typically vary according to the level of activity and may limit one’s participation in sports. As problems progress, patients may also lose speed and strength, and notice swelling. The condition is increasingly common in middle age. For reasons unknown, it occurs most in women, and may begin as early as the teenage years. It has even been suggested that some people may be predisposed to chondromalacia. Women suffer most from this condition possibly due to muscle weakness in the extension mechanism and anatomical factors, which cause the kneecap to slip out of alignment. Symptoms may be especially severe with repetitive activities like running or aerobics, although cyclists are not immune to the problem.
Arthritis and Degenerative Joint Surfaces
Just like the chrome on a trailer hitch can get pitted with age, so can the joint surfaces become pitted and damaged in the knee joint. When this happens, the friction can be excruciatingly painful. Typically, when this becomes severe, joint replacement is the last option. But this is a major surgery, and because of the lifespan of an artificial joint is only about 15 to 20 years, this option is held out for those who can’t respond to other treatment options. Arthritis literally means “fire in the joints.” People who suffer from the disease can attest to the accuracy of this description. Statistics from the Arthritis Foundation estimate that one in seven Americans is affected. Many are elderly, but arthritis is not a disease which discriminates according to age. It affects every strata of the population, young and old, women more so than men. Osteoarthritis is the most common form of arthritis and makes a particularly strong showing in the middle aged. The term osteoarthritis is synonymous with “wear and tear” arthritis, or degenerative joint disease. The terms refers to the actual wear and erosion of the articular cartilage, which continues until finally no cartilage remains and bone rubs against bone. Symptoms include pain, stiffness, and swelling. At first they may be intermittent, but as deterioration progresses, they occur with greater regularity and intensity. When the entire thickness of the articular cartilage has worn away and bone rubs harshly against bone, pain increases dramatically and may be incapacitating.
The tendency to develop osteoarthritis is often inherited. Other factors include injury or repetitive stress from excessive use. Those who are bowlegged or have knock-knees are at increased risk. The last, but perhaps the most common factor is excess body weight.
Arthritis: Osteoarthritis
This is a degenerative joint disease stemming from wear and tear on the knee usually affecting those in middle age and older. Osteoarthritis causes the cartilage to erode away. Symptoms include pain, stiffness, and swelling that at first happens once in a while but can progress to chronic pain.
Arthritis: Rheumatoid Arthritis
Rheumatoid arthritis is a second form of arthritis. Instead of a process of wear and tear, it begins with inflammation, which eventually leads to destruction of one or many joints. Its cause is unknown. It affects all age groups, but most often attacks women in middle age. It may attack a single joint, but more commonly simultaneously attacks many joints within the body.
The disease manifests itself in many ways. In some cases the symptoms involve one or two joints, are transient, and vanish without causing permanent damage. More commonly, many joints are affected, rapid deterioration occurs, and joints become grossly deformed. Both large and small joints may be damaged. The knee is often affected along with other large joints such as the hips.
Arthritis: Crystaline Arthritis
Inflammation of the joints can occur when a small granual of sodium urate (related to gout) or calcium phosphorate (related to chondrocalsinosis) gets lodged in the joint. The effect is similar to getting a piece of sand trapped in your eye. It irritates the surrounding inflammation. Middle-aged men are most prone to this sort of arthritis.
Pre-Patellar Bursitis
Pre-patellar bursitis involves the bursae sacs on the front of the kneecap. Bursae are fluid-filled sacs that are found throughout the body in areas where the skin must glide over bones. They help to minimize friction. One of the jobs of bursae in the knee is to enable the kneecap to move about freely underneath the skin. When pressure is placed on the knee from either a direct blow or from kneeling repetitively, problems can arise.
For example, this problem in the past was also called “housemaid’s knees,” because often those women who scrubbed floors on hands and knees suffered from this knee problem. Similarly, brick masons, carpet layers, and electricians are also afflicted. At times the condition occurs when the bursal sac becomes infected, often for reasons which are not readily apparent. Regardless of the cause of inflammation, pain and swelling can be present in front of the kneecap.
A rubbery, bulging mass in front of the kneecap that may feel sore and tender, can develop. Except in the case of infection, treatment consists of relieving pressure. Kneeling is avoided or only performed with knee pads. The good news is that only in persistent cases is surgery necessary.

 Chronic pain
Chronic pain