- Locations
- Find a Physician
- By Physician
- By Department
- The Center for Spine Health
- Hand & Wrist Center
- Shoulder & Elbow Center
- Foot & Ankle Center
- Joint Replacement Center
- The Sports Medicine Center
- Pediatric Orthopedic Center
- Trauma & Fracture Center
- Osteoporosis and Bone Health
- Oncology Center
- Cartilage Repair Center
- Concussion Rehab Center
- OrthoDirect
- Careers
- Patient Portal
- Intranet
Arthritis is a common condition that can affect all joints in the human body. Arthritis results in the loss of the smooth cartilage surface that covers the ends of a bone in a joint. In addition, arthritis can result in deformity of the joint surfaces. When this occurs in the shoulder (glenohumeral joint) patients experience pain, loss of motion, and functional limitations. The most common form is osteoarthritis.
 Osteoarthritis is associated with wear and tear and aging. Genetic factors likely have a role in the development of shoulder osteoarthritis. Other causes of arthritis include previous shoulder dislocations and surgery, traumatic joint injury such as a fracture, chronic massive rotator cuff tearing, inflammatory diseases such as rheumatoid arthritis, avascular necrosis, and some other very uncommon causes. Although arthritis is often considered a common joint problem, arthritis of the shoulder is less uncommon than arthritis of other large joints such as the knee and hip. Arthritis can affect the glenohumeral (ball and socket) and the acromioclavicular joints of the shoulder.
Osteoarthritis is associated with wear and tear and aging. Genetic factors likely have a role in the development of shoulder osteoarthritis. Other causes of arthritis include previous shoulder dislocations and surgery, traumatic joint injury such as a fracture, chronic massive rotator cuff tearing, inflammatory diseases such as rheumatoid arthritis, avascular necrosis, and some other very uncommon causes. Although arthritis is often considered a common joint problem, arthritis of the shoulder is less uncommon than arthritis of other large joints such as the knee and hip. Arthritis can affect the glenohumeral (ball and socket) and the acromioclavicular joints of the shoulder.
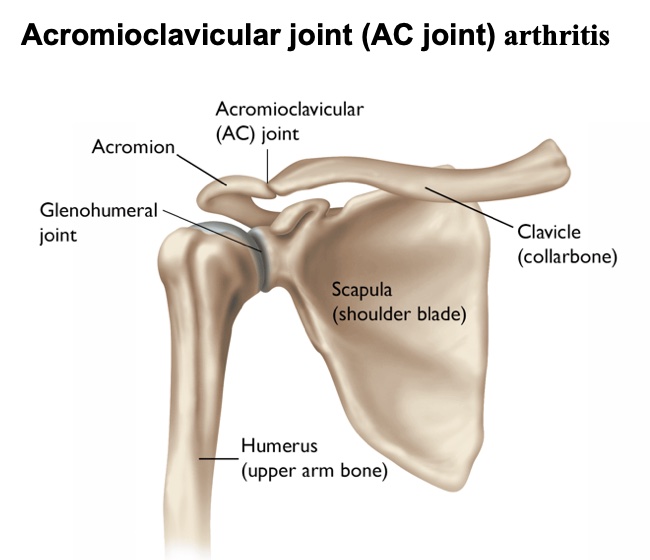 Acromioclavicular Joint Arthritis
Acromioclavicular Joint Arthritis
The acromioclavicular joint (AC joint) is a small joint between the clavicle and acromion (a bony projection from the scapula).
The joint is surrounded by strong ligaments and has very little motion. Although there is very little motion at the AC joint, it is a very important supporting structure of the shoulder girdle. The acromioclavicular joint suspends the entire shoulder and upper extremity from the trunk. Although the acromioclavicular joint is commonly affected by arthritis, it is not always painful. Many individuals with a painless, normal functioning shoulder have evidence of AC arthritis on x-rays.
AC joint arthritis affects a broad age range. In younger patients it is commonly associated with sports or work activities such as weight lifting or heavy labor. In many cases the arthritis and symptoms develop without an injury or specific cause. With advancing age, AC joint arthritis is commonly associated with rotator cuff disorders. Isolated AC arthritis can also occur. Less commonly, an acromioclavicular joint sprain or separation can lead to the later development of acromioclavicular joint arthritis.
The pain is usually localized at the end of the clavicle but can also radiate into the front of the shoulder or into the upper trapezius muscle toward the neck. In many cases there is a firm swelling or prominence at the end of the clavicle and acromioclavicular joint. Pain is worsened when reaching across the chest, reaching behind the back, or when lying on the affected shoulder. The diagnosis is usually evident on regular x-rays. In some cases of inflammation of the joint, without obvious x-ray findings, the diagnosis can be confirmed with MRI.
Many cases can be treated with anti-inflammatory medications, cortisone injections, and activity modification. In occasional cases, surgery is performed to remove the end of the clavicle where it meets the acromion. This surgery is usually performed with arthroscopic techniques.
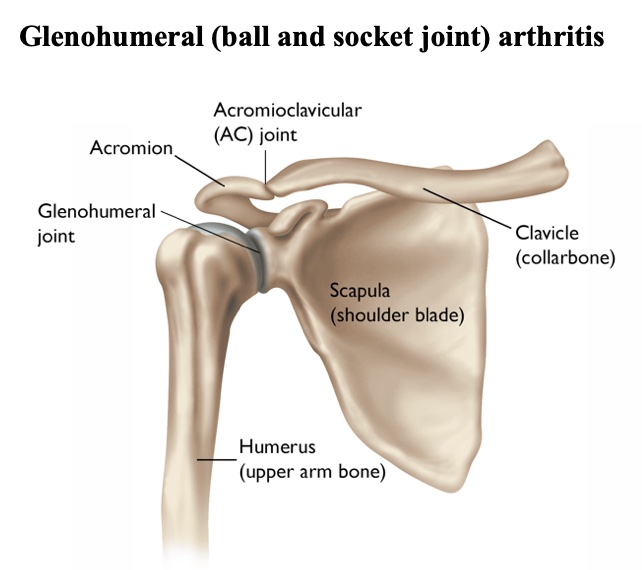
Glenohumeral (ball and socket joint) arthritis
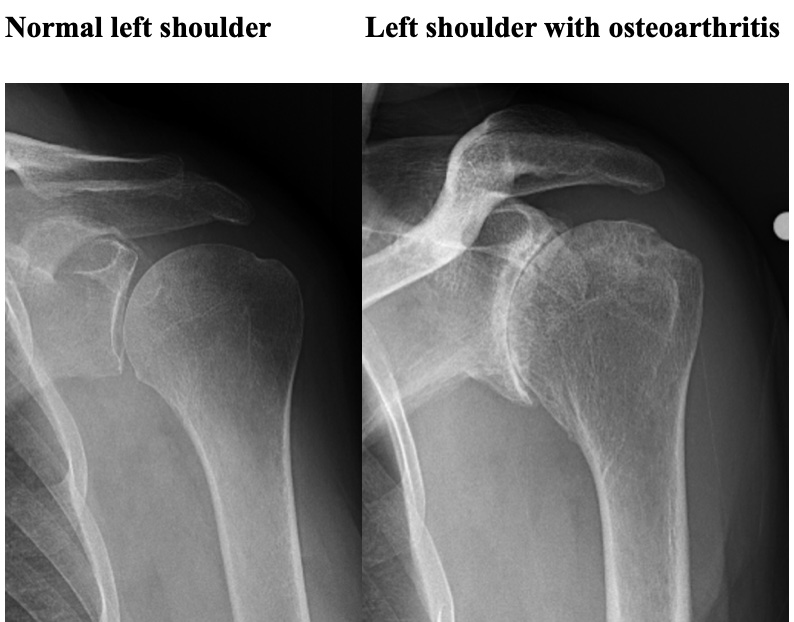
Osteoarthritis is the most common form of arthritis. Compared to hip and knee arthritis, osteoarthritis of the glenohumeral joint (the ball and socket of the shoulder) is less common. It usually presents in patients after age 55. Less commonly it presents in younger patients as a result of excessive use (i.e. weight lifting, and heavy labor), after prior surgery for shoulder dislocations, or severe shoulder fractures.
Osteoarthritis results in the gradual destruction of the articular cartilage of the humeral head and glenoid. This is usually a gradual process that occurs over the course of many years. In addition, the normal shape of the spherical (round) humeral head and matching glenoid socket are lost. The earliest sign of glenohumeral osteoarthritis is shoulder pain and mild loss of shoulder motion. In many cases, early osteoarthritis is confused with shoulder impingement syndrome and rotator cuff disorders. In most cases the diagnosis is easily determined with appropriate x-rays of the shoulder.
The initial treatment of glenohumeral osteoarthritis consists of activity modification, stretching exercises to restore and maintain shoulder motion, and oral anti-inflammatory medications. Cortisone injections can provide symptomatic relief but should not be the mainstay of treatment. Viscosupplementation with hyaluronic acid is also an option that is not currently FDA approved for treatment of shoulder disorders but is approved for knee injection. Viscosupplementation in the shoulder can be effective for temporary relief of symptoms, but this is an off-label use and usually not covered by insurance. Other substances can be injected, such as PRP (platelet rich plasma) or stem cells but there is no strong evidence that these substances are effective.
When non-operative treatment fails, and the symptoms are intolerable, surgery is indicated. In some milder cases arthroscopic surgery to release scarring and clean out arthritic debris can successfully reduce pain and improve function. Arthroscopic surgery is usually not helpful when there is advanced symptomatic glenohumeral osteoarthritis. In addition, arthroscopic surgery does not remove arthritis or prevent the progression of the disorder. In some cases arthroscopic surgery can worsen the symptoms.
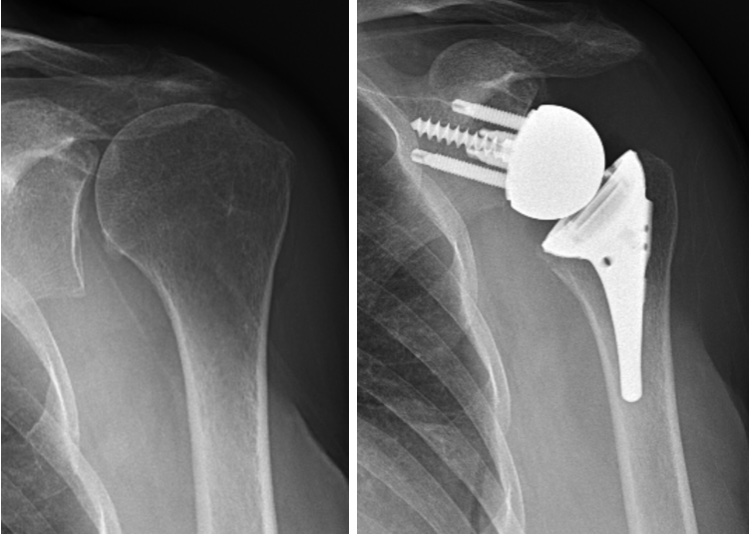
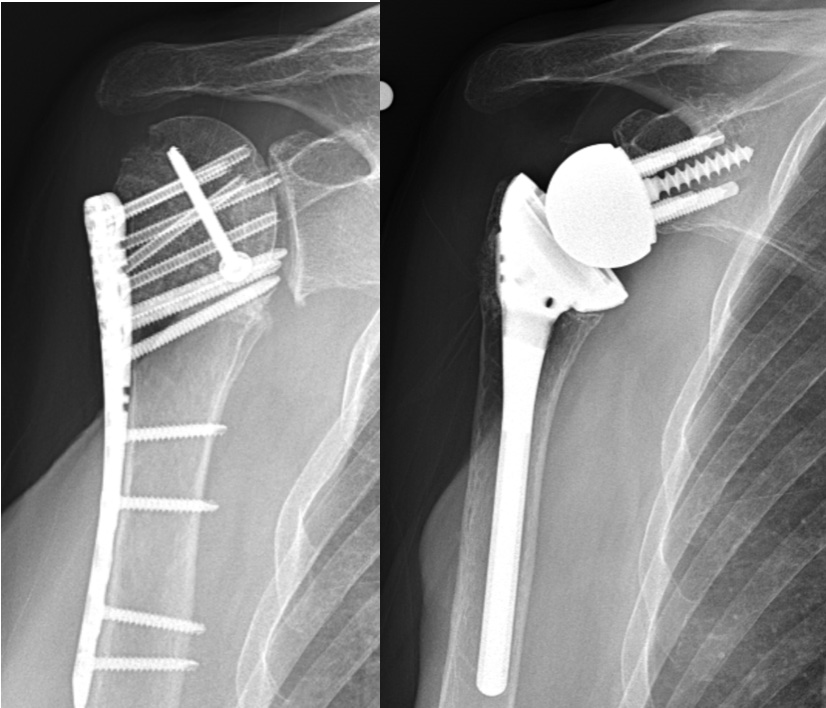
Shoulder replacement is indicated when there is advanced glenohumeral osteoarthritis. Most patients undergo replacement surgery because of shoulder pain. Shoulder replacement is similar in concept to hip replacement. The humeral head is replaced with a metallic implant. Anatomic total shoulder replacement includes replacement of the glenoid socket as well as the humeral head with implants that mimic the normal anatomy.
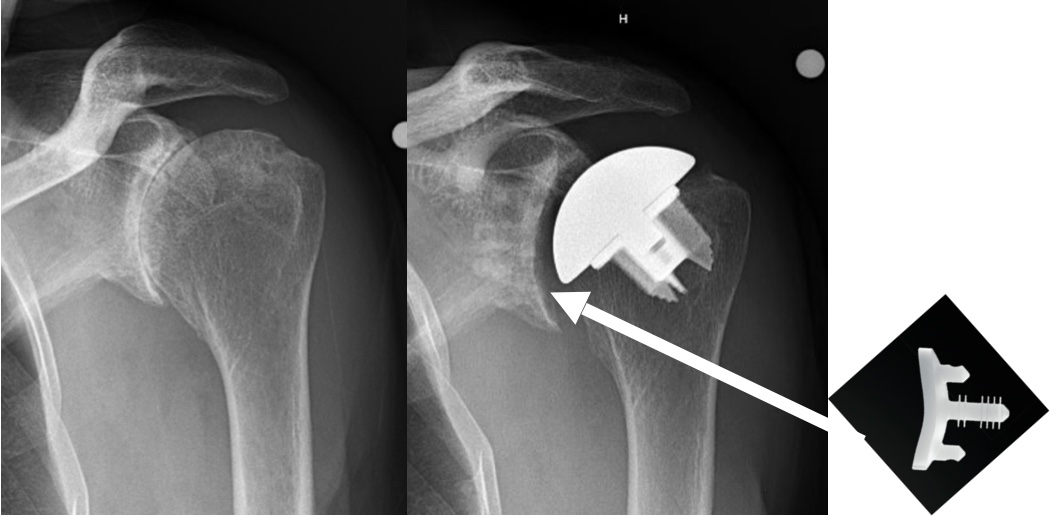
Anatomic total shoulder replacement requires a good rotator cuff. The replacement glenoid is made of plastic (ultra high molecular weight polyethylene). While most severely arthritic shoulders require glenoid replacement, there are occasional cases that can be treated with a humeral head resurfacing or a humeral head replacement can be performed. The ream and run procedure with a humeral head replacement and smoothing of the glenoid is an option for physically active, often younger patients, who want to participate in heavy physical activities and avoid the potential problems associated with anatomic glenoid replacement. The are some patients with osteoarthritis who have severe glenoid bone deformities and/or rotator cuff tearing who are treated with a reverse total shoulder. Reverse total shoulder was developed for the treatment of shoulder with severe rotator cuff tears. More recently, use of reverse total shoulder has expanded to some osteoarthritic shoulders. This is currently considered an off-label use of reverse total shoulder.

Shoulder replacement is a fairly extensive surgical procedure. However, the recovery is often less difficult that patients expect. It can often be performed with an interscalene/brachial plexus nerve block in conjunction with general anesthesia. This anesthetic technique provides better post-operative pain relief and avoids some of the potential complications of deep general anesthesia. Active and healthy patients with good home support and care can have outpatient shoulder replacement surgery. Other patients may stay in the hospital for one night. It is rare for a patient to require transfer to an inpatient rehabilitation facility instead of being discharged to their home. An arm sling is worn for 4 to 6 weeks after surgery.
The post-operative rehabilitation, goals, and outcome are dependent on the extent of shoulder damage. Although most patients have excellent pain relief, patients with a good rotator cuff tend to have better functional outcomes. Shoulder motion exercises are begun the day after surgery. It is critically important for patients to do their exercises. Stiffness or limited motion is a difficult problem to overcome, but is very preventable. Strengthening is not formally emphasized until there is good shoulder motion. Many patients have substantial pain relief within a couple of weeks after surgery. Most patients are very functional with activities of daily living at 3 months after surgery. The end result is usually achieved by 1 year after surgery. The reported rate of patient satisfaction is greater than 95 percent.
The complications of shoulder replacement surgery include but are not limited to infection, nerve injury, bleeding, stiffness, persistent pain, instability, bone fracture and loosening or failure of the replacement parts, future need for revision surgery, as well as anesthetic and medical complications that are associated with all surgery. Complications are rare and there are a number of steps that are taken to help prevent them.
Rotator Cuff Tear Arthropathy
Rotator cuff tear arthropathy is a combination of massive unrepairable rotator cuff tear and glenohumeral arthritis. Many patients can be treated with activity modification, stretching exercises to restore and maintain shoulder motion, strengthening exercises, and oral anti-inflammatory medications. Cortisone injections can provide symptomatic relief.
When non-operative treatment fails to provide adequate pain relief and functional improvement shoulder replacement is an option. An anatomic humeral head replacement or humeral resurfacing can be performed in patients who are able actively (independently) raise their arm above their shoulder and have good strength. In most cases a reverse total shoulder replacement is performed to relieve pain and restore shoulder function.
Left shoulder with massive Left shoulder treated with reverse total shoulder rotator cuff tear and rotator cuff tear arthropathy
A reverse total shoulder replacement is specifically designed to be used in cases that do not have a functioning rotator cuff. The implants include a metal hemisphere that is attached to the glenoid/scapula and a metal humeral implant that has a plastic (polyethylene) socket.
 Post-traumatic arthritis
Post-traumatic arthritis
Glenohumeral arthritis can occur after a fracture of the proximal humerus (upper end of the arm bone). This is more common after surgical treatment of fractures. These fractures can damage the blood supply to the proximal humerus causing avascular necrosis and joint damage. The hardware used to treat a fracture can also damage the joint.
Rheumatoid Arthritis
Rheumatoid arthritis is a systemic inflammatory disease that causes joint destruction. The shoulder is commonly involved to varying degrees. Rheumatoid arthritis affects all of the joint tissues including the articular cartilage (joint surface), ligaments, rotator cuff tendons, and surrounding muscles. Early involvement is treated or controlled with medical management. This is typically directed and monitored by a rheumatologist.
Early surgical management can involve arthroscopic synovectomy and debridement. Occasionally, rotator cuff repair without joint replacement is indicated if the joint surfaces are still intact. In some cases, the rotator cuff tear is so large that it cannot be repaired.
Shoulder replacement is indicated when the symptoms can no longer be adequately controlled with medical management. The results of earlier replacement are generally better than late replacement. Patients with a significant rotator cuff or bony involvement may be a candidate for a reverse total shoulder replacement.
Avascular Necrosis
Avascular necrosis (AVN) is a relatively uncommon cause of shoulder arthritis. The most common causes are corticosteroid (prednisone) used to treat other diseases such as asthma, chronic pulmonary diseases, rheumatologic diseases, cancer, and organ transplantation. In addition, AVN can result from a shoulder fracture. The blood supply to the humeral head (ball) is damaged which can lead to collapse of the humeral head bone and destruction of the cartilage surface. This can eventually cause severe joint destruction. In early cases, before there is joint damage, non-operative treatment can maintain function. Drilling of the humeral head (core decompression), similar to surgery performed for hip avasular necrosis, can be performed before there is joint collapse. When there is joint collapse and damage a shoulder replacement is the best treatment to provide pain relief and functional restoration. It is better to perform a replacement before there is extensive collapse of the humeral head and destruction of the glenoid.
Andrew Green, MD
Professor of Orthopaedic Surgery
Chief of Shoulder and Elbow Surgery
Warren Alpert Medical School, Brown University