- Locations
- Find a Physician
- By Physician
- By Department
- The Center for Spine Health
- Hand & Wrist Center
- Shoulder & Elbow Center
- Foot & Ankle Center
- Joint Replacement Center
- The Sports Medicine Center
- Pediatric Orthopedic Center
- Trauma & Fracture Center
- Osteoporosis and Bone Health
- Oncology Center
- Cartilage Repair Center
- Concussion Rehab Center
- OrthoDirect
- Careers
- Patient Portal
- Intranet
Understanding Fracture Prevention
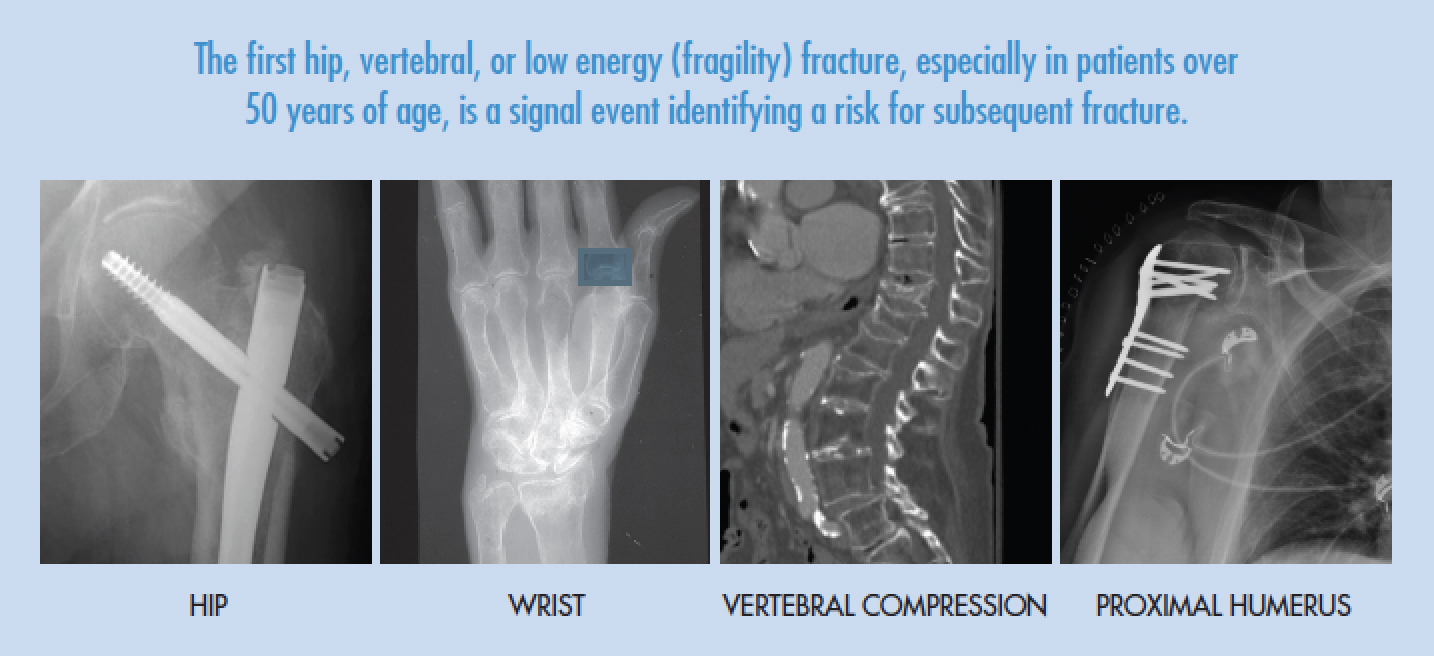
Individuals who suffer a hip or spine fracture, or a fracture caused by minimal injury (low energy or, “fragility” fracture) are at risk of experiencing subsequent fractures. Fractures, particularly in individuals over 50 years of age, can result in disability, deformity, loss of independent living, and premature death.
Appropriate medical intervention can reduce the risk of subsequent fractures in individuals who have suffered a fracture and it is recommended that all patients, especially those over 50 years of age, with low energy, hip, and spine fractures be evaluated and treated.
Treatments are now available to prevent further bone loss and in many cases to restore bone strength. This reduces the risk of subsequent fractures.
Evaluation
Secondary fractures can occur even with normal bone density.
The evaluation of fracture risk, and risk reduction, includes:
- Medical history focused on bone health
- Physical examination including gait, balance and strength assessment
- Measurement of bone density by DEXA scan
- Assessment of fracture risk
- Blood and urine tests of osteoporosis
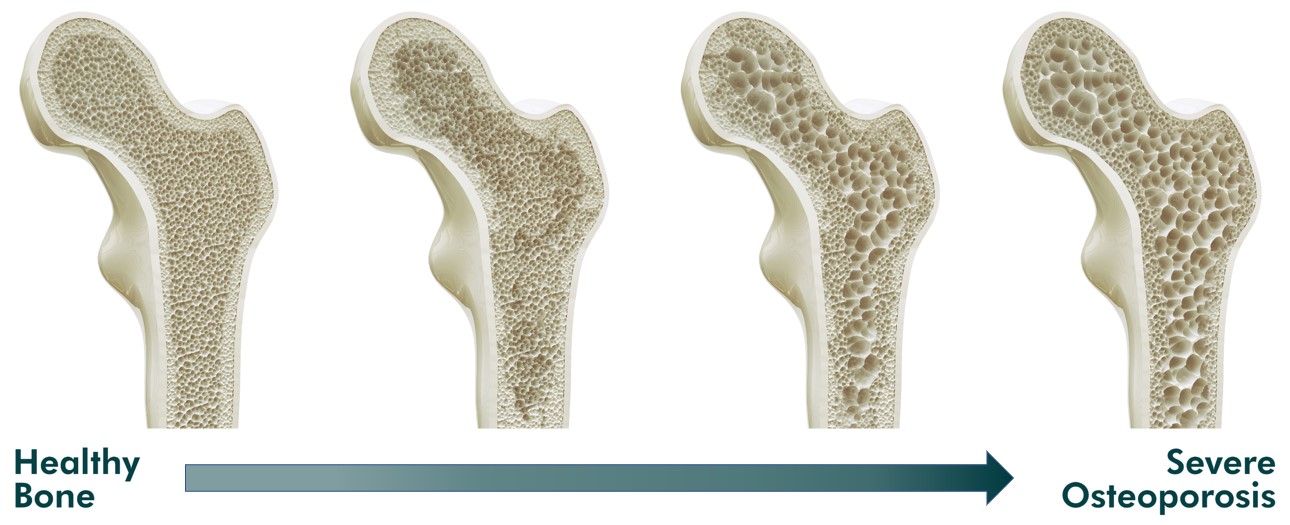
Analyzing Bone Density
Bone mineral density or bone strength, is measured with a type of low energy x-ray called a DEXA scan. The scan is entirely noninvasive and takes approximately 15 minutes to complete. The measurement of an individual’s bone mineral density is compared to values of the normal population to determine the extent of bone loss. Patients under active treatment should have follow-up DEXA scans at 1-2 year intervals.

Estimation of the Risk of Subsequent Fractures
Information obtained from the medical evaluation, DEXA scan, and laboratory tests make it possible to estimate the risk of subsequent fractures. We are using an online computerized assessment program called FRAX. FRAX is the World Health Organization’s fracture risk assessment measurement which provides a risk assessment reflecting specific personal features.
Treatment Options
Treatment is individualized for each patient depending upon individual needs.
- Often dietary, lifestyle, and activity counseling are sufficient to reduce the risk of subsequent fractures.
- Medical history, physical examination, and laboratory tests can establish risk factors needing particular treatment.
- Medications to build bone strength and reduce fracture risk.
- Gait, balance, and strength training can reduce the risk of falls.
- Follow-up visits with annual DEXA scans are important to assess the effectiveness of treatment.
What to Do
After a fracture, especially one resulting from minimal trauma, or other indications of decreased bone strength such as hip and spine fractures, you should consult the Metabolic Bone/Fracture Prevention Service.
For Providers
Older people who have suffered a hip or vertebral fracture, or low energy (fragility) fractures, are at extremely high risk of another fracture yet a majority of them do not receive appropriate evaluation or treatments following their fracture.
The recommendations for evaluation and treatment to prevent secondary fractures represent the consensus of a broad multi-stakeholder coalition assembled by the American Society for Bone and Mineral Research Secondary Fracture Prevention Initiative and endorsed by multiple organizations including the Agency for Healthcare Research and Quality, the National Institute of Arthritis and Musculoskeletal and Skin Diseases, the National Institute on Aging, the National Osteoporosis Foundation, the American Academy of Orthopedic Surgeons, American Orthopedic Association, and the US Bone and Joint Initiative, among 35 other international groups.
The recommendations define the target population and recommend clinical actions that should be taken to diminish the risk of, and protect patients from, secondary fractures.
The recommendations are based upon:
1.The recognition that the first hip, vertebral, or low energy (fragility) fracture, especially in patients over 50 years of age, is a signal event, identifying a risk for subsequent fracture.
2. A fracture is a multi-factorial event and half of hip, vertebral, fragility, and stress fractures occur in individuals with normal bone density as measured by dual energy X-ray absorptiometry (DEXA) scan.
3. The decision for treatment includes DEXA as one important criterion but depends on the entire clinical evaluation, not solely on the bone mineral density.
4. Low bone density does not always indicate osteoporosis but includes:
- Hyperparathyroidism
- Osteomalacia
- Renal osteodystrophy
- Hematologic malignancies
Patients for whom Evaluation is Appropriate
1. Greater than age 50 years with a fracture as a result of a ground level fall/low energy trauma.
2. Fragility or stress fractures: vertebral compression, hip, pelvic ring, proximal humerus, distal radius, and low energy ankle fractures.
3. Patients with osteopenia who are planning elective total joint replacement.
4. A history of reduced bone density or use of medication known to be associated with bone loss and osteoporosis: proton pump inhibitors, selective serotonin reuptake inhibitors, opioids, anticonvulsants, immune modulators, aromatase inhibitors, glucocorticoids.
5. Concern for low bone density, or risk for secondary fracture including:
- Secondary osteoporosis including, prominently, the endocrine disorders, hyperparathyroidism, hypercortisonism, hyperthyroidism, diabetes, and hypogonadism.
- Rheumatoid arthritis, lupus, liver and kidney disease, inflammatory bowel disease, bariatric surgery, and chronic obstructive pulmonary disease.
- A variety of other conditions including premature menopause, anorexia nervosa, athletic amenorrhea, multiple sclerosis, immobilization and impaired mobility, and alcohol abuse.
Services Provided
1. Medical history focused on bone health
2. Physical examination including gait, balance, strength, and fall risk assessment
3. Measurement of bone density by DEXA scan and FRAX fracture assessment
4. Metabolic bone laboratory tests including bone turnover markers
5. Preoperative bone health optimization prior to elective procedures (e.g. joint replacement, spine)
6. Counseling on diet, dietary supplements, medications, activity, lifestyle, optimizing the home environment to reduce the risk of falls
7. Medications to build bone strength and reduce fracture risk:
- Dietary supplementation as needed including protein, vitamin D, and calcium
- Antiresorptives and osteoanabolics
8. Physical therapy exercise programs for gait and balance training to prevent falls
Referral to the Metabolic Bone/Fracture Prevention Service
To refer a patient, please call 401-274-9660, option #2, with patient’s first and last name and date of birth.
1. There will be no change in your follow-up appointment routine with patient.
2. The typical Metabolic Bone/Fracture Prevention Service patient schedule consists of:
- Visit 1: History and physical exam; DEXA scan; Labs as needed.
- Visit 2: Follow-up on labs; institution of pharmacotherapy or other interventions as appropriate.
- Visit 3: Follow-up to ensure safety and comfort of medications and serum calcium monitoring.
- Visit 4: One-year follow-up for annual DEXA to assess treatment efficacy.